Introduction
Kidney transplant of human being is a modern technique in this era. Kidney transplantation is often the preferred treatment for those with end-stage renal disease. The discipline of kidney transplantation has grown tremendously over the past 50 years. Patients with end-stage renal disease have better long-term survival if they are placed on the waiting list and eventually undergo kidney transplantation than those who stay on dialysis.
Furthermore, those who undergo transplantation often experience a better quality of life and a projected survival benefit of 10 years over those who remain on dialysis. Since kidney transplantation was first successfully performed by Dr. Joseph Murray in 1954, there have been major developments in transplantation and immunology, allowing for a wider selection of acceptable donors and recipients.
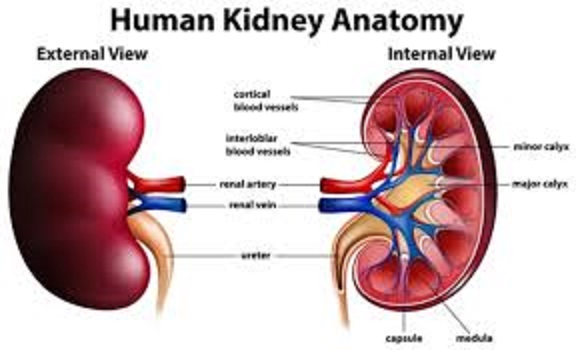
Anatomy and physiology
Before Kidney transplantation it is very necessary to understand the anatomy of kidney. The kidneys are two bean-shaped organs located in the lower back, one on each side of the spine. They play a crucial role in maintaining overall health through various functions:
Anatomy:
1. Cortex: The outer layer of the kidney, containing nephrons (functional units).
2. Medulla: The inner layer, containing renal pyramids and calyces.
3. Nephrons: Tiny units consisting of glomeruli (capillaries) and renal tubules.
4. Glomeruli: Capillary clusters filtering blood.
5. Renal tubules: Tubes reabsorbing water, electrolytes, and nutrients.
6. Ureters: Tubes connecting kidneys to the bladder.
7. Renal arteries and veins: Blood vessels supplying and draining the kidneys.
Physiology:
1. Filtration: Glomeruli filter waste, excess fluids, and electrolytes from blood.
2. Reabsorption: Renal tubules reabsorb water, electrolytes, and nutrients.
3. Secretion: Tubules secrete waste products, like urea, into the filtrate.
4. Excretion: Waste products are excreted in urine.
5. Regulation of electrolytes and fluids: Kidneys maintain homeostasis by adjusting electrolyte and fluid levels.
6. Acid-base balance: Kidneys help maintain acid-base balance by excreting excess hydrogen ions.
7. Blood pressure control: Kidneys regulate blood pressure through fluid balance and hormone secretion.
8. Erythropoiesis: Kidneys produce erythropoietin, stimulating red blood cell production.
9. Vitamin D activation: Kidneys convert vitamin D into its active form.
The kidneys work together to:
– Remove waste products
– Regulate electrolyte and fluid balance
– Maintain acid-base balance
– Control blood pressure
– Produce hormones
– Support red blood cell production
Understanding kidney anatomy and physiology is essential for appreciating their vital role in maintaining overall health.
Indications
Indications for kidney transplantation:
1. End-Stage Renal Disease (ESRD): Irreversible kidney failure requiring dialysis or transplantation.
2. Chronic Kidney Disease (CKD): Advanced CKD with significant loss of kidney function.
3. Acute Kidney Injury (AKI): Severe kidney damage requiring transplantation.
4. Recurrent Kidney Disease: Repeat episodes of kidney disease or failure.
5. Congenital Kidney Abnormalities: Birth defects affecting kidney function or structure.
6. Nephrotic Syndrome: Excessive protein loss in urine leading to kidney damage.
7. Glomerulonephritis: Inflammation of kidney filters (glomeruli) causing kidney damage.
8. Diabetic Nephropathy: Kidney damage due to diabetes.
9. Hypertensive Nephrosclerosis: Kidney damage caused by high blood pressure.
10. Polycystic Kidney Disease (PKD): Genetic disorder causing cysts on kidneys.
11. Kidney Cancer: Removal of a kidney due to cancer, with transplantation of the remaining kidney.
12. Other Rare Kidney Diseases: Certain rare conditions, such as Fabry disease or oxalosis, may also require transplantation.
Note: Each case is evaluated individually, and transplantation may be considered for other indications not listed here.
Patient Selection
Patient selection for kidney transplantation involves evaluating potential recipients to ensure they are suitable candidates for the procedure. Key factors considered:
1. Medical history: Overall health, kidney disease severity, and co-existing conditions.
2. Age: Typically, 18-70 years old, but may vary depending on individual health.
3. Kidney function: Level of kidney impairment and need for dialysis.
4. Tissue typing: Matching recipient and donor tissue types to minimize rejection risk.
5. Cross-matching: Ensuring no antibodies against the donor kidney.
6. Infection screening: Ruling out active infections that could compromise the transplant.
7. Cancer screening: Ensuring no active cancer that could impact the transplant.
8. Cardiovascular evaluation: Assessing heart health to ensure it can withstand the procedure.
9. Psychological evaluation: Assessing mental fitness and support system.
10. Lifestyle habits: Evaluating smoking, alcohol use, and other habits that may impact the transplant.
11. Social support: Ensuring a strong support system for post-transplant care.
12. Financial stability: Ensuring ability to cover ongoing medical expenses.
13. Compliance: Assessing willingness to adhere to post-transplant medication and care.
A multidisciplinary team reviews these factors to determine the patient’s suitability for kidney transplantation.
Donor Selection
Donor selection for kidney transplantation involves evaluating potential donors to ensure they are suitable and healthy enough to donate a kidney. Key factors considered:
1. Age: Typically, 18-65 years old, but may vary depending on individual health.
2. Medical history: Overall health, kidney function, and absence of diseases.
3. Blood type: Matching blood type with the recipient.
4. Tissue typing: Matching tissue type with the recipient to minimize rejection risk.
5. Cross-matching: Ensuring no antibodies against the recipient’s tissue.
6. Kidney function: Ensuring adequate kidney function in the donor.
7. Urinalysis: Normal urine test results.
8. Imaging studies: Normal kidney anatomy and function on imaging tests.
9. Infection screening: Ruling out active infections.
10. Cancer screening: Ensuring no active cancer.
11. Psychological evaluation: Assessing mental fitness and willingness to donate.
12. Family history: Assessing genetic risk factors.
13. Lifestyle habits: Evaluating smoking, alcohol use, and other habits.
14. Blood pressure and cardiovascular health: Ensuring good blood pressure control and cardiovascular health.
15. Surgical risk assessment: Evaluating the risk of surgical complications.
Donors can be:
– Living related donors (family members)
– Living unrelated donors (friends, partners)
– Deceased donors (after brain death or cardiac death)
The evaluation process ensures the donor’s safety and the best possible outcome for both the donor and recipient.
Treatments
Types of kidney transplant
1. Living Donor Transplant: A kidney is donated by a living person, usually a family member or friend.
2. Deceased Donor Transplant: A kidney is donated by someone who has passed away.
3. Paired Exchange Transplant: A living donor donates a kidney to a recipient, and in return, the recipient’s original donor donates to another person.
Process of Kidney Transplant
The process of kidney transplantation involves several steps:
Pre-Transplant
1. Evaluation: Recipient and donor evaluation, including medical history, blood tests, and imaging studies.
2. Matching: Matching donor and recipient blood type, tissue type, and cross-matching.
3. Scheduling: Scheduling the transplant surgery.
Transplant Surgery
1. Donor nephrectomy: Removing the donor kidney.
2. Recipient preparation: Preparing the recipient for surgery.
3. Implantation: Implanting the donor kidney in the recipient.
4. Vascular anastomosis: Connecting blood vessels.
5. Ureteral anastomosis: Connecting the ureter to the bladder.
Post-Transplant
1. Recovery: Monitoring the recipient in the ICU and hospital.
2. Immunosuppression: Starting immunosuppressive medications.
3. Follow-up: Regular follow-up appointments with the transplant team.
4. Lab tests: Regular lab tests to monitor kidney function and medication levels.
5. Lifestyle modifications: Adhering to a healthy lifestyle, including diet and exercise.
Living Donor Process
1. Donor evaluation: Evaluating the living donor’s medical history and kidney function.
2. Donor surgery: Removing the donor kidney using laparoscopic or open surgery.
3. Donor recovery: Monitoring the donor’s recovery.
Deceased Donor Process
1. Donor identification: Identifying a deceased donor match.
2. Donor procurement: Recovering the donor kidney.
3. Transportation: Transporting the donor kidney to the recipient’s location.
Note: The process may vary depending on the transplant center and individual circumstances.
Side Effects Of Kidney Transplant
Kidney transplant surgery can have various side effects, including:
1. Rejection: The body may reject the new kidney, which can be acute or chronic.
2. Infections: Increased risk of infections, especially in the first year after transplant.
3. Medication side effects: Immunosuppressive medications can cause:
– Nausea and vomiting
– Diarrhea or constipation
– Fatigue
– Hair loss
– Mood changes
– Increased risk of cancer
4. Surgical complications: Bleeding, blood clots, or wound infections.
5. Kidney damage: The new kidney may be damaged during surgery or due to rejection.
6. High blood pressure: Common after kidney transplant.
7. Diabetes: Some immunosuppressive medications can increase the risk of developing diabetes.
8. Bone disease: Long-term use of immunosuppressive medications can lead to bone loss or osteoporosis.
9. Anemia: Iron deficiency or other factors can cause anemia.
10. Mental health concerns: Anxiety, depression, or stress related to the transplant process.
11. Gastrointestinal issues: Nausea, vomiting, diarrhea, or stomach pain.
12. Sexual dysfunction: Hormonal changes or medication side effects can affect sexual function.
13. Sleep disturbances: Difficulty sleeping or insomnia.
14. Nutritional deficiencies: Malabsorption or dietary restrictions.
15. Financial burden: Transplantation and ongoing care can be costly.
It’s essential to discuss these potential side effects with your transplant team to understand the risks and benefits and develop strategies for managing them.
Precautionary Measure for Kidney transplant
To minimize risks and ensure a successful kidney transplant, take the following precautionary measures:
1. Careful donor selection: Ensure the donor kidney is compatible and healthy.
2. Thorough recipient evaluation: Assess the recipient’s overall health and suitability for transplant.
3. Infection control: Implement strict infection control measures during surgery and post-transplant care.
4. Immunosuppressive medication management: Closely monitor and adjust medication to prevent rejection and minimize side effects.
5. Regular follow-up: Schedule regular check-ups with the transplant team to monitor progress and address concerns.
6. Lifestyle modifications:
– Maintain a healthy diet
– Engage in regular exercise
– Avoid smoking and alcohol
– Manage stress
7. Medication adherence: Strictly follow the medication regimen to prevent rejection.
8. Vaccinations: Stay up-to-date on recommended vaccinations to prevent infections.
9. Avoid excessive sun exposure: Reduce skin cancer risk due to immunosuppressive medications.
10. Pregnancy planning: For female recipients, plan pregnancies carefully to ensure optimal outcomes.
11. Travel precautions: Take necessary precautions when traveling, such as carrying a transplant card and maintaining medication schedules.
12. Dental care: Practice good oral hygiene and schedule regular dental check-ups to prevent infections.
13. Mental health support: Access support for emotional well-being and stress management.
14. Financial planning: Prepare for ongoing transplant-related expenses.
15. Education and support: Stay informed and connected with the transplant team, support groups, and resources.
By taking these precautionary measures, you can minimize risks and ensure a successful kidney transplant experience.
2 thoughts on “Kidney Transplant”